FlyingMed - Smart and Secure Drone-Delivered Naloxone System for Opioid Overdose Treatment
Overview
The US is in the midst of an unprecedented opioid crisis in which 130 people lose their lives from an opioid overdose (OD) each day. These are particularly tragic events because they often affect young people, many of whom could be rescued by early administration of naloxone antidote which comes in an FDA approved nasal spray form that can be given by a lay bystander. Despite programs making the antidote publicly accessible and availability of training on its use, <5% of bystanders witnessing an opioid OD actually administer naloxone to the victim, either because it is unavailable or they don’t know how…or are afraid…to use it on their own. An opioid OD kills by causing the victim to stop breathing and, within a couple of minutes, if not reversed by the antidote, the heart stops beating resulting in death. Once this occurs, the chances of survival decline approximately 10% per minute. (3) It is often not physically possible for first-responders to reach the victim and administer the antidote quickly enough to save their life once they stop breathing. The most efficient urban Emergency Medical Services (EMS) systems in the US and throughout the world may get to the curb in an average of 8-10 min (longer in suburban or rural areas) after 9-1-1 dispatch, but it typically takes several more minutes for them to reach the victim, do an initial assessment, and administer medication. (4, 5) Sadly, it is often too late to save the victim. The challenge of saving more opioid overdose victims comes down to time. Data from a recent NIH sponsored study involving paramedics from 55 top EMS agencies in 10 cities showed the median time from the call to 9-1-1 until first drug administration in a cardiac arrest patient (similar EMS response as an opioid OD) was 16 minutes (roughly 18 minutes from when the patient stopped breathing), and the situation gets even worse in suburban and rural areas, where service is often provided by volunteer fire first responders and paramedics, and the travel distances and time intervals are much longer. Our proposed solution to mitigate this crisis is to develop, optimize, and test a novel drone-delivered naloxone system that will provide more rapid delivery of the antidote to opioid overdose faster than traditional EMS and guide the lay responder on how to administer the naloxone via real time audio/video direction.
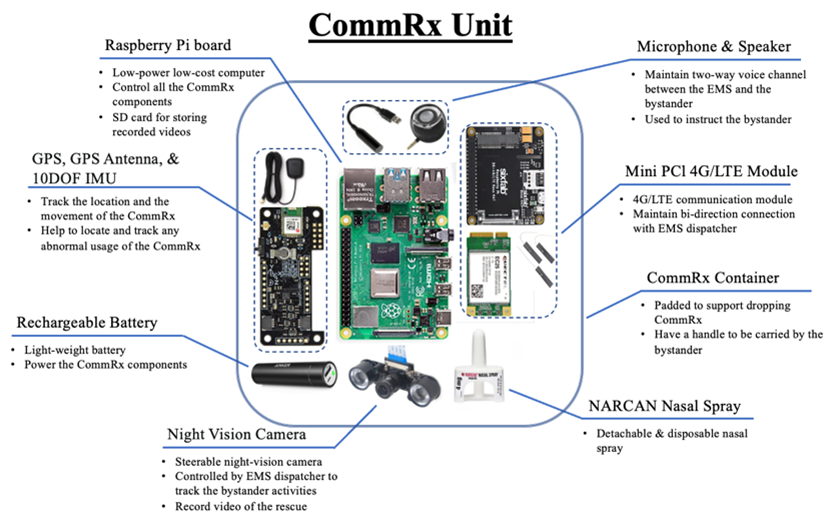
The ultimate goal of our envisioned operational system is to provide extremely rapid launching and ≤2 min delivery (from 9-1-1 first responder dispatch) of naloxone antidote to a bystander caller’s. Our flight tests from our preliminary works confirmed the need to use a faster drone than those we initially tested to deliver naloxone to a caller in an average of 2 minutes after drone launch. We set this goal so approximately 50% of callers would receive and administer the naloxone spray to the victim before EMS curb arrival. We chose these performance specifications to achieve a clinically meaningful increase in the % of victims who could be treated before EMS arrival while keeping the number of drone installations and costs as affordable as possible. In addition, there are several modifications or additions will be necessary over our earlier preliminary work. For example, we need to make some changes to address challenges with densely populated urban areas such as Richmond city. The route planning and pre-mission payload delivery area identification may need to be done differently in our urban areas when responding to a multilevel building. We summarize the research tasks that we intend to address in this project as: i) development of detachable CommRX supporting faster drones, ii) develop optimal flying routes and FAA on-board Remote-ID module, iii) development of a two-way authentication mechanism, iv) development of a pinpoint delivery logistics to identify the exact dropping point of the bystander caller, and finally, v) train and evaluate the performance of our developed system.
People
Faculty
PhD Students
- Mohammed Ayyat
Funding
- National Institute of Health (NIH)/National Institute on Drug Abuse (NIDA) 1R41DA051293-01
Any opinions, findings, and conclusions or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the views of the National Science Foundation.